Two months ago, a new patient named Shamizu came to the clinic. She is a young and lovely girl who has been living in Japan for many years. She had a large lipoma on her chest and I think she found me through the internet. Interestingly, she is also a blogger and she wrote a blog post about her experience of finding me for lipoma surgery. The post was so vivid and interesting, like a live broadcast, and she immediately sent it to me to read. I also share with you some of our interactions and viewpoints on that day.

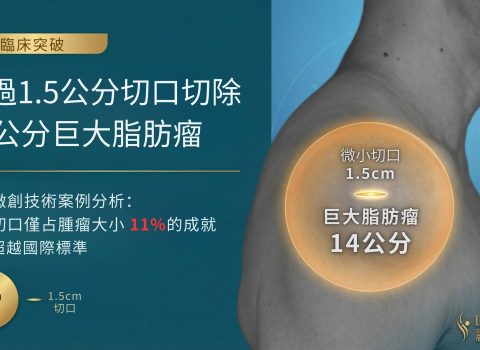
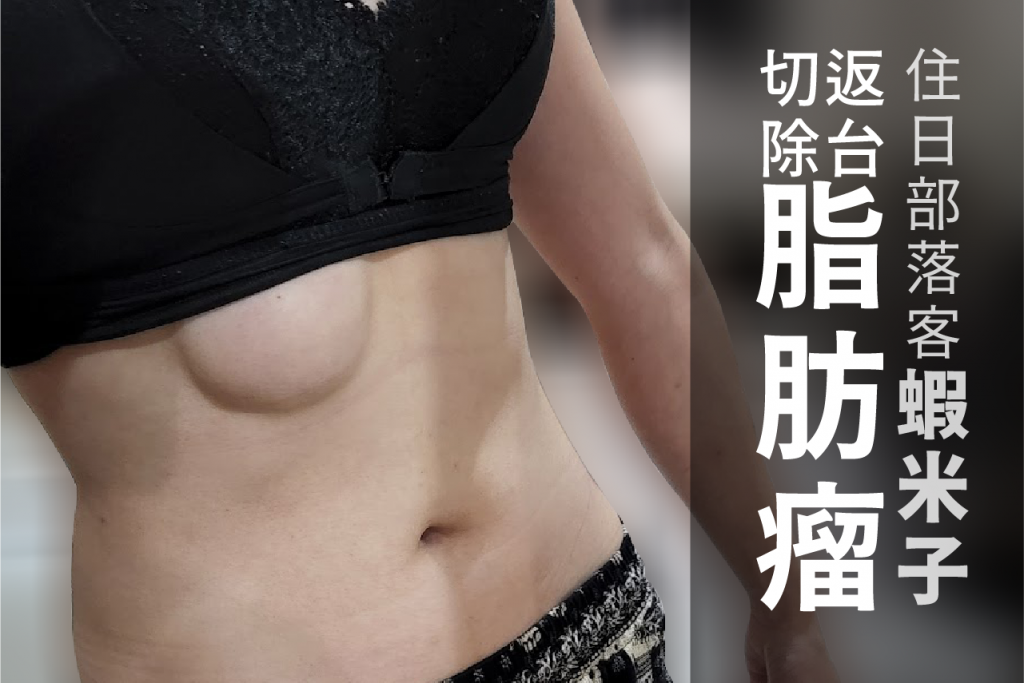
I remember that on the day of the consultation, Shamizu’s lipoma was located under her left chest like a round ball hiding under the skin. If it wasn’t called a lipoma, it actually looked quite cute. Because she is very thin, the lipoma looked particularly prominent. I think it may be easy to attract attention when wearing half-length tops or swimsuits.
According to her observation, she accidentally found a small bump under her left chest two years ago. She was worried that it was cancer, but later found out that it was a common lipoma, so she decided to observe and not treat it for the time being. One year later, she found that the lipoma had grown and was being compressed by her bra. She also had an ultrasound at a hospital in Japan at that time, but the doctor told her that the lipoma was deep and there was a risk of damaging the internal organs during surgery, so she needed to go to a larger hospital. She was scared and didn’t dare to have the surgery in Japan. She was also worried that taking leave from work for hospitalization would affect her job, so she could only continue to observe it. Another year passed, and the lipoma grew larger, causing pain when she exerted force. The lump had compressed the nerves, so she finally decided to take leave and return to Taiwan for surgery, and she came to me.
In fact, Shamizu’s situation is similar to that of other patients. Generally, when patients come for consultation in the early stages of lipoma, the lump is still small (because lipomas cannot grow overnight, haha). Usually, when people discover a polyp or lump, they will first do research online or have a preliminary medical examination. If the examination result is not a malignant tumor, there is no pain or pressure, and it does not affect daily life, most people will choose to observe it, and even doctors will suggest not to have surgery.
As long as it is judged to be a benign tumor and the lump is not necessarily going to continue to grow, it is okay to observe it. Because surgery is not like taking medicine or getting injections, it requires a more complicated process, and postoperative care and recovery time are needed. Even for people who have never had surgery, they may not have a sense of security, and they may not trust the doctor’s skills too much. If there is no impact on daily life and it is not necessary, more than 90% of people should choose not to have surgery.

My opinion is different. Lipoma surgery is already a routine surgery for me, just like having meals every day. In the case of being very familiar with this kind of surgery, I suggest removing it as soon as possible. What I consider for patients is not only the impact on their daily life, but also that I want them to have a confident smile. If it is a technique that I am very familiar with, and I am very confident that I can handle it after examination, why not suggest to my patients to have surgery? Early surgery can minimize the wound and there is no need to wait for the lipoma to grow. If you have a lipoma, other doctors may say, “Oh, you can choose surgery to remove it, but it doesn’t affect your life. Just keep observing if it grows.” But I will say, “Oh, it won’t affect your life, but surgery can handle it right away without waiting for it to grow.”
I would not recommend taking chances with lipomas and betting that they won’t grow, unless the risk of surgery is very high and I cannot fully control the condition. Otherwise, I think there is no need to endure the agony of time. Moreover, while the lipoma is still small, the surgery time is fast, the wound is small, it is easy to take care of postoperatively, and the scar is small, so you don’t have to worry about dealing with the scar later.
I have encountered many patients with huge lipomas, over 10 cm, who have gradually become accustomed to living with the lump over time. Some people have even caused great inconvenience in their lives. After enduring for a long time, they finally came to me with anxiety to solve their problem. After solving it, they really feel relieved and happy from the bottom of their hearts.
Related reading:
- Surgical Record of a 19.5 cm Giant Lipoma – Unloading My 15-Year Backpack
- Surgical Removal of a 15 cm Back Lipoma
Shamizu’s surgical experience and thoughts are described wonderfully in her blog. I think it is a good reference for people who have lipomas but have not yet had surgery or for those who have just had surgery and are in the process of recovery.
Shamizu’s Surgical Record
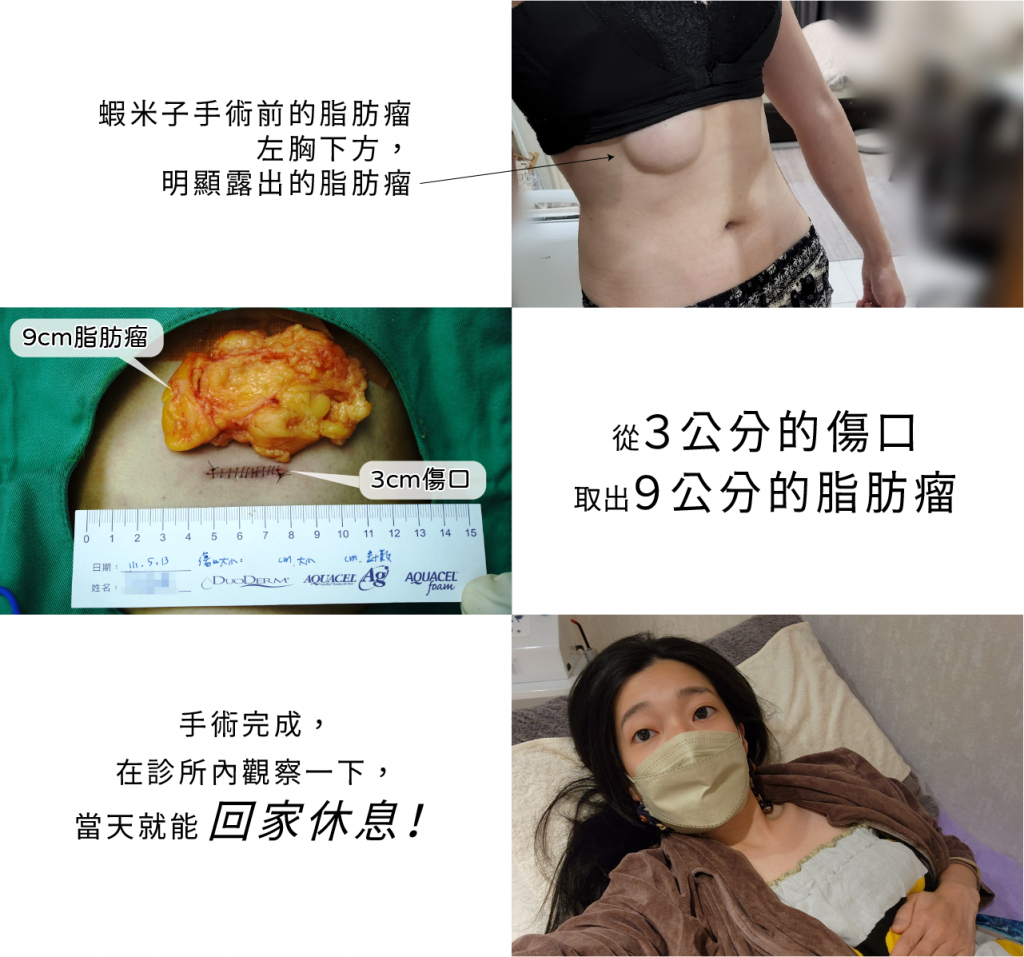
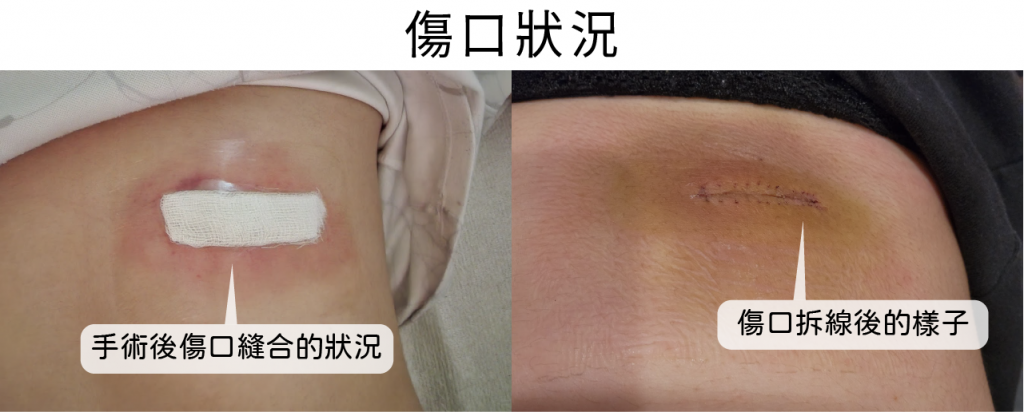

Lipoma removal surgery is a general outpatient surgery. The surgery takes less than an hour to complete, and patients can go home to rest on the same day. However, the key is the patient’s understanding of lipoma surgery and their confidence in the doctor. As a doctor, I can provide the most suitable advice based on my expertise, but ultimately, the decision on how to face the situation still lies with the patient.
Regarding lipomas, it is essential to know that they are benign tumors composed of adipose tissue. They usually grow slowly and have no symptoms. In most cases, lipomas do not require treatment. However, if they become painful, infected, or start to affect a person’s daily life, surgery may be necessary.
In conclusion, it is essential to observe lipomas, but it is equally important to consult a doctor for advice. Early surgical intervention can minimize the wound’s size and hasten the healing process. Patients should seek medical attention if they experience pain, discomfort, or any other adverse symptoms.
For more information about lipomas and surgical procedures, please refer to the following link: Lipomas – Lius Clinic.